Some recent investigations have focused on the interactions between various neurohumoral and pharmacologic mechanisms. Combined neurohumoral influences may serve to augment or inhibit smooth muscle contraction.
Some recent investigations have focused on the interactions between various neurohumoral and pharmacologic mechanisms. Combined neurohumoral influences may serve to augment or inhibit smooth muscle contraction.
There are several interactions between the histamine (Hi)-receptor and the autonomic nervous system. In addition to being one potential stimulant of the afferent vagal irritant receptor, a nonreflex synergism between electrical stimulation of the vagus nerve and exogenously administered histamine has been reported in dogs.
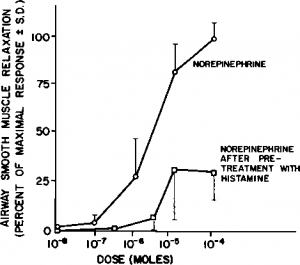
Histamine may also serve to augment bronchoconstriction through sympathetic interactions. We have shown that pretreatment with histamine diminishes the beta-adrenergic relaxation response to exogenous norepinephrine in dogs (Fig 3). Other investigators have suggested possible alpha-adrenergic augmentation of histamine-induced contraction in human airways.
Intracellular Metabolism of Airway Smooth Muscle
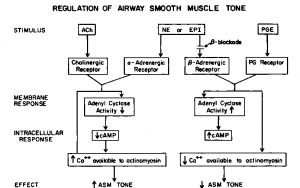
Bronchomotor tone is ultimately regulated bythe availability of intracellular calcium to the contractile apparatus of the respiratory smooth muscle cell. Sequestration of calcium, either intra- or extracellularly, results in diminished contractility while increased availability of calcium augments muscle contraction. Many investigations have focused upon the role of 3′, 5′-cyclic adenosine monophosphate (cAMP) in this process. Intracellular cyclic nucleotides modulate contraction by controlling intracellular calcium availability. Promotion of cAMP synthesis through activation of the enzyme, adenyl cyclase, leads to sequestration of calcium, and the contractility of airway smooth muscle is diminished (Fig 4).
Figure 4 is a schema of the interactions of various agonists with the cAMP system. Beta-adrenergic agonists and certain prostaglandins promote the activation of cAMP. Beta-adrenergic agonists may also act independently of the cAMP system to promote calcium sequestration. In contrast, alpha- adrenergic and cholinergic stimulation serve to inhibit cAMP synthesis. Direct augmentation of calcium sequestration by acetylcholine has also been postulated. Corticosteroids augment the bronchodilator effects of beta-adrenergic drugs, but this effect is much less rapid than the relaxation effects of beta-angonists. The mechanism by which corticosteroids augment muscle relaxation is not known. Potentiation either at the beta-receptor on the cell membrane (leading to increased adenyl cyclase activation) or promotion of calcium sequestration within the cell may be important The cAMP-system is not the mechanism, however, by which muscle contraction or relaxation is mediated, but rather a modulating system for augmenting or inhibiting contractile stimuli. The adenyl cyclase-cAMP system is thus another homeostatic mechanism in the regulation of bronchomotor tone.
adrenergic and cholinergic stimulation serve to inhibit cAMP synthesis. Direct augmentation of calcium sequestration by acetylcholine has also been postulated. Corticosteroids augment the bronchodilator effects of beta-adrenergic drugs, but this effect is much less rapid than the relaxation effects of beta-angonists. The mechanism by which corticosteroids augment muscle relaxation is not known. Potentiation either at the beta-receptor on the cell membrane (leading to increased adenyl cyclase activation) or promotion of calcium sequestration within the cell may be important The cAMP-system is not the mechanism, however, by which muscle contraction or relaxation is mediated, but rather a modulating system for augmenting or inhibiting contractile stimuli. The adenyl cyclase-cAMP system is thus another homeostatic mechanism in the regulation of bronchomotor tone.
Summary
1. Asthma is a syndrome rather than a single disease with bronchoconstriction as the final common pathway.
2. Allergy is not an essential component of the asthmatic response; however, it remains uncertain if mediators are an essential component of most asthmatic responses.
3. The sympathetic nervous system appears to play a minor role in the homeostatic control of bronchomotor tone. Direct innervation of airways by sympathetic nerves appears to play virtually no role in bronchodilation in humans. Adrenal secretion of epinephrine may be a more significant physiologic factor in promoting bronchodilation.
4. The mechanism by which beta-blockade causes bronchoconstriction in asthmatic subjects but not normal subjects is unclear. Recent work suggests that this may result from either unmasking of the alpha-adrenergic constrictor response (which is not adrenal dependent) or from unopposed cholinergic constrictor tone.
5. The role of the cholinergic (parasympathetic) nervous system appears to be central to nonatopic asthmatic bronchoconstriction. Asthma may occur from reflex vagal stimulation of afferent irritant receptors.
6. Histamine may have many other functions in the bronchoconstrictor response. Histamine causes airway smooth muscle contraction, but this is not significant in normal human subjects or in most canine models. However, considerable variability in responsiveness to histamine exists among both normal human subjects and many animals. Furthermore, histamine responsiveness may be augmented by efferent vagal output and, possibly, by alpha-adrenergic stimulation. Histamine also antagonizes ^-adrenergic relaxation of airway smooth muscle.
7. Ultimately, intracellular calcium availability determines the magnitude of the contractile response. Cyclic adenosine monophosphate appears to play a role in calcium regulation, although some neurohumoral effect on calcium sequestration probably occurs independently of the cAMP system. Contrary to earlier speculations, the adenyl cy-clase-cAMP system serves to modulate rather than to mediate respiratory muscle contraction.
Figure 3. Effect of histamine on bronchodilator response of norepinephrine in a canine model. There is substantial reduction in airway relaxation after pretreatment with histamine. This may result from physiologic antagonism of the beta-adrenergic relaxing response of from alpha-aug-mentation of histamine response.
Figure 4. Modulation of bronchomotor tone by cyclic adenosine monophosphate. Beta-adrenergic agonists and prostaglandins act to promote cAMP synthesis and calcium sequestration. With less Ca available to the contractile apparatus of die cell, die contractile response is modified or abolished. Alpha-adrenergic and cholinergic stimulation act antagonistically at the cell membrane to lower cAMP concentrations in the cell and hence to promote contractility. Direct effects on Ca sequestration are also proposed in this schema. (Adapted from discussion and diagrams of C. Schultz.)
All mentioned references earlier:
Pathogenesis of Asthma: Introduction
Pathogenesis of Asthma: Theories of Asthma Pathogenesis